Premiums for Affordable Care Act insurance plans will see relatively modest increases averaging 3.6 percent next year, and some states will actually see rate decreases, according to an analysis released Friday by the consulting firm Avalere and the Associated Press.
Every county in the country will have at least one provider, the report said, and 19 states will have either new insurers entering their markets or see existing insurers expand their coverage.
Premium increases in the individual marketplaces established by the 2010 health care law averaged 30 percent this year.
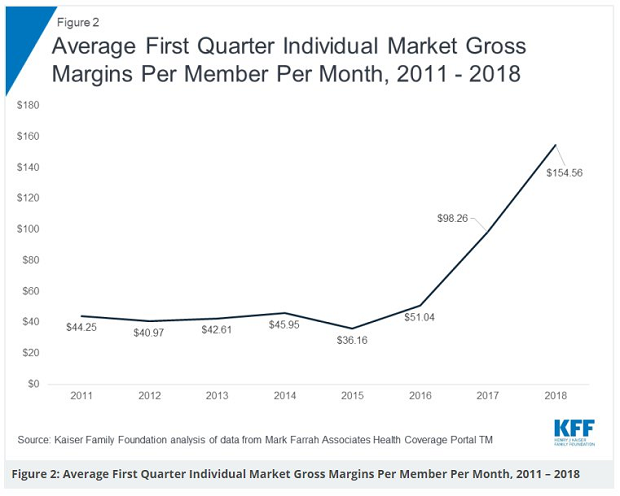
Why premiums aren’t rising as sharply: Insurers raised rates dramatically last year amid considerable political uncertainty, leaving them less room to raise prices this year, given Obamacare’s requirement that they spend at least 80 percent of premium revenue on paying medical claims. “Insurers are very profitable right now in the individual market following previous increases that overshot what was needed, so they can't justify big increases,” Larry Levitt of the Kaiser Family Foundation tweeted, along with this chart showing the sharp increase in gross margins for ACA plans over the last two years.
Why it matters: The ACA “health insurance marketplaces seem to be stabilizing after two years of sharp premium hikes,” the AP said. “And the exodus of insurers from the program has halted, even reversed somewhat, with more consumer choices for 2019.”
But even as ACA markets stabilize, cost is still an issue. The average monthly premium for an Obamacare plan is now nearly $600 a month, too high for many middle-class customers who earn too much to receive federal assistance. “This is still a market that’s unaffordable for many people who aren’t eligible for subsidies,” said Avalere’s Chris Sloan.
Even so, the relative health of the ACA marketplaces comes as a surprise to some, given President Trump’s efforts to subvert the system. “It's quite remarkable how resilient the ACA has been in the face of efforts by Congress and the Trump administration to undermine it,” Levitt said. “If not for repeal of the individual mandate penalty by Congress and expansion of loosely-regulated short-term plans by the Trump administration, it's quite possible that average ACA premiums would be going down in 2019.”