If anything good is to come from the Ebola obsession currently infecting the country, it might arise from reporters and public officials taking a close look at the state of the public health system in the U.S. That’s not because Ebola poses a threat to the public at large, but because there are plenty of viruses that do, and in the event of an outbreak, it might be a little late to realize that our public health infrastructure has been starved of funds for the better part of a decade.
To be clear, even in the event of a widespread epidemic of, say, a severe strain of influenza, there is no suggestion that the public health system in the U.S. could collapse the way systems in Liberia, Sierra Leone, and Guinea have.
Of the 5,723 registered U.S. hospitals, this report deals with the 1,248 federal, state and local government hospitals that were affected by budget cuts during the recession. Still, that’s 22 percent of the total—mostly in vulnerable, low income areas. A bare minimum of functionality probably isn’t the bar we ought to be aiming to clear.
Related: Ted Cruz Says Obama’s Public Health Officials Can’t Be Trusted on Ebola
Unfortunately, as a recent report issued by the Association of State and Territorial Health Officials shows, state-level budget cuts have been eating away at the capacity of state health agencies since the onset of the Great Recession in 2008.
“SHAs continue to experience budget cuts and job losses, resulting in the reduction or elimination of critical public health programs and services,” the report found. “Critical SHA programs and services have been cut or reduced, staff positions have been eliminated and many staff have been laid off or furloughed.”
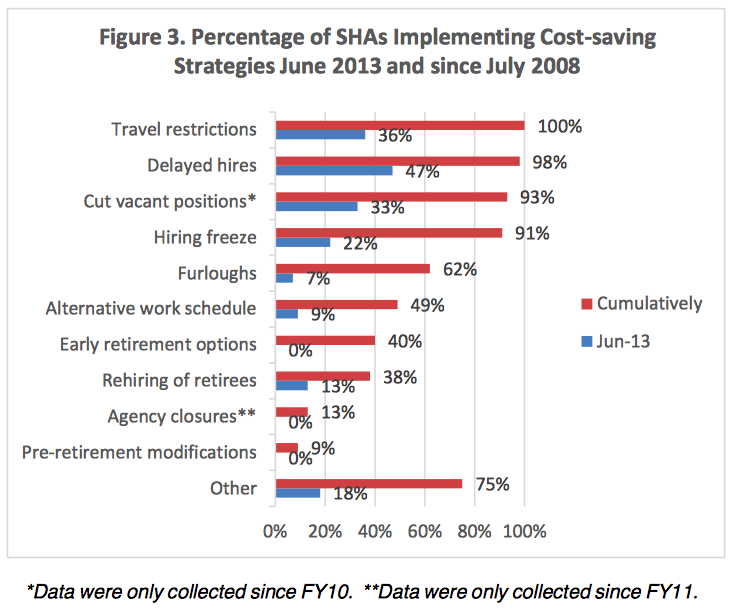
State-level health agencies, like many state functions were frequently subject to budget cuts during the recession and in the years that followed. By 2013, according to ASTHO data, 100 percent of their members had implemented travel restrictions, and virtually reported various kinds of staffing reductions, including hiring freezes, involuntary furloughs, elimination of vacant positions, and delayed hiring of vacant positions.
The result has been the elimination or curtailment of various kinds of programs. For instance, the state of Georgia “has limited the scope of services provided for genetic testing, diagnosis, counseling, and management for children, along with care coordination and other needed medical and health services for children and youth with chronic conditions,” the report said.
Related: Ebola Czar’s First Challenge Is Calming the Public
The situation is just as critical, if not more so, at the state and local level – the first line of defense against an epidemic. The National Association of County and City Health Officials, local health departments across the country lost 44,000 jobs between 2008 and 2013. And NACCHO found that funding for emergency preparedness programs was typically one of the first victims of budget cuts.
The cuts to individual agencies, according to the Institute of Medicine, come at the same time that efforts to plan and coordinate responses to widespread public health crises have been neglected.
If the U.S. does face a public health crisis, the report said, that’s very bad news. “These planning efforts are essential,” it read, “because, absent careful planning, there is enormous potential for confusion, chaos, and flawed decision making in a catastrophic public health emergency or disaster.”
Top Reads from The Fiscal Times
- Ad Spending in the Next 16 Days Could Decide the Senate
- Social Safety Net Lifted 39 Million Out of Poverty in 2013
- Businesses Upbeat About Jobs, Economic Growth




