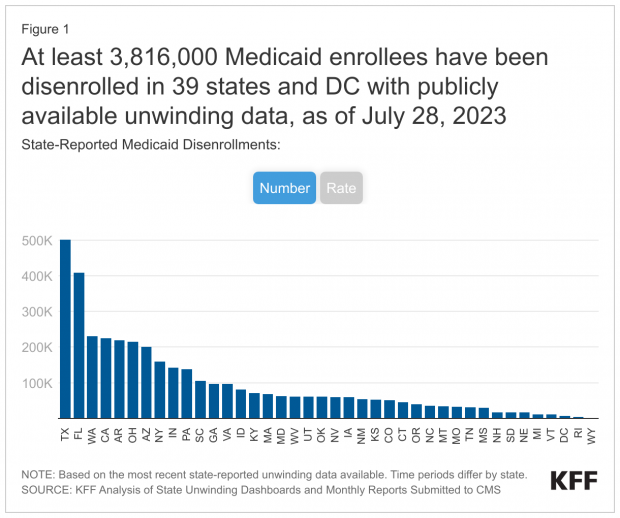
More than 3.8 million Americans across 39 states and the District of Columbia have been removed from Medicaid since April after the expiration of a pandemic-era provision ensuring that they could keep their coverage throughout the health emergency.
KFF, a health policy group tracking disenrollment data, says that the number undercounts the actual number of people who have lost Medicaid coverage — and that 73% of all people who have been cut off from the program had their coverage terminated for procedural reasons not related to whether or not they were still eligible for Medicaid. “High procedural disenrollment rates are concerning because many people who are disenrolled for these paperwork reasons may still be eligible for Medicaid coverage,” KFF says.
In the eight states reporting age data, children account for 32% of Medicaid disenrollments, according to KFF.
Kristin Fortner, identified as a 33-year-old waitress in Arkansas earning $3 an hour plus tips, is quoted in The Washington Post describing her efforts to navigate the bureaucratic maze involved in reapplying for coverage after being cut off from Medicaid at the end of April: “It’s very, very frustrating,” Fortner told the Post’s Amy Goldstein. “I keep thinking I’ve done everything I’m supposed to do and it’s fine, but then, when I check, it’s not fine.”